Posts by Laura Reeves
573 – Search and Rescue Titling Events Come to US
Search and Rescue Titling Events Come to US
Melissa Stagnaro, vice president of the American Rettungshunde Sport Association (ARSA), joins host Laura Reeves to share details of the growing Search and Rescue Sport titling events in the US.

Dog working in an ARSA test.
“ARSA started out of a need for some standardizations,” Stagnaro said. “There was an earthquake and flooding in Armenia in the late 1980s and a lot of kind-hearted people showed up to help and it was hard to ascertain what their skill level was. This included search and rescue dog handler teams, but it also included EMT’s and nurses and people like that. And so sometimes the well-intentioned helpers caused a little more trouble than help.
“So the United Nations worked with the FCI and out of this came an International Rescue dog organization. And so the rule book that we’re using is standard across the globe. Most countries, other than the US, use this as their basis for their local community SAR teams.”
ARSA offers these tests as a way for people to do titling events that could, if they stick with it and find their dog has the aptitude and they have the aptitude, take them to the point that they could do full on search and rescue missions.
“There’s three sport levels that get progressively more difficult, and there’s a fourth mission ready level,” Stagnaro said. “So the mission ready, if you and your dog were to complete it successfully, you would be a real search and rescue team certified by the FCI rulebooks. The three other levels are just sport.
“There’s a lot of search and rescue community-based groups in the US and also sheriff’s departments who would be more interested in accepting a volunteer that already has the skills. In the US we have many certifications for search and rescue teams, but if you came to them and said, hey look, my dog already has these skills, then they would have an easier time assessing you. None of the sport skills are in conflict with real search and rescue.”
The ARSA 2023 Championship is March 31 – April 1 in Leesburg, VA.
Listen in to the full episode for more details on this fun new sport.
Team Subkit: The Voice Of Purebred Dogs | Pure Dog Talk
Thanks to Team Subkit for the invite. Interested in starting your own entrepreneurial journey in dogs but unsure what to expect? Then read up on our interview with Laura Reeves,…
Read Full Post572 – Dog Food Behind the Scenes: Meat, Meal and Byproducts Defined
Dog Food Behind the Scenes: Meat, Meal and Byproducts Defined
Rob Downey, nutritionist, researcher and CEO of Annamaet dogfood company, joins host Laura Reeves for a deep dive on what ingredients lists on our dog food labels mean.
“We have to back up a little bit and look at what those statements mean and where definitions come from,” Downey said. “That really comes from AAFCO. You’ll see on the package whether it be canned, frozen or whatever. AAFCO is Association of American Feed Control Officials. They don’t regulate pet foods. What they do is they set up the guidelines. And then the regulation goes through the FDA and the Department of Agriculture in most states. So AAFCO is actually a volunteer organization. Each person gets a vote, and you have to be on one of these bodies. So each state has the ability to regulate how they view it. And the sad part is, those regulations are open to the interpretation of each state official. So, every state has a feed control official. And as a pet food manufacturer, for me to sell in each state, I have to be approved by that state. So, you have to send your labels in to each individual state.
“They are the ones that determine the terminology that we’re allowed to use. And so, for example, fresh meat. If the meat you use has been frozen at any time, it’s no longer considered fresh. So as a manufacturer, I wouldn’t trust shipping non-frozen meat. What I call fresh meat, I want frozen and I’ll thaw it when I want to use it, but then I can’t attach the word fresh to it.
“Then you get into the term meal, and meal is actually a processing term where you take raw meat, and it’s heated up, moisture is removed, a lot of the fats removed and it becomes a powder and then that’s how it shipped as a meal. And then that’s also called a rendered ingredient. AAFCO is pretty strict about rendered. Anytime you change the physical component or whatever, you heat it up or you do this or do that now, it becomes a rendered product. So even in the food chain, like for instance my local meat store, if they make a sausage? If it was in the pet industry, that would be considered rendered
And the other thing that is kind of interesting, the term meal isn’t used in most parts of the world. Like if I use chicken meal, somebody in Europe, they don’t have the term meal. They would call it dehydrated chicken or simply chicken.
“Now the advantage of using a meal, is that basically the moisture has been removed. So, if I’m ordering chicken meal, a truckload, it’s only going to be 10% moisture. I’m ordering fresh chicken, a truckload is going to be 70% water, only 30% dry matter. But when you read the label. On the ingredient list, it’s according to wet weight, so it includes all that water. That’s why when you see a fresh meat formula or a meat formula, there’s always seems to be more meat ingredients, because there’s so much water. Of course, when you’re doing an extruded product that all gets kicked out.
“So chicken meal is basically skin, muscle and no internal organs. Like you can’t have organ meat in it, you can have some bone in it. But when you go to byproduct meal, that’s when the organ meat gets involved.”
Mind Blown…
When the label gives the minimum percentages of the contents (30/20 protein and fat, for example), it doesn’t have to specify the maximum, which can vary drastically from the minimum! Listen in for more insider details.
571 – Skin is Your Dog’s Largest Organ, Keep it Healthy!
Skin is Your Dog’s Largest Organ, Keep it Healthy!
Dr. Marty Greer, DVM joins host Laura Reeves for a deep dive on skin problems in our dogs, how to avoid them, what causes them and how to treat them.
Pro Tip? An ounce of prevention is worth a pound of cure.
In previous episodes, Marty and Laura discuss allergies and external parasites, but today’s topic covers hot spots, seasonal alopecia, demodex and other skin disorders.
“The skin, believe it or not, is the largest organ of the body,” Greer noted. “So, it accounts for an important part of our dog’s health and it accounts for a huge number of visits. A lot of people have noticed skin problems in their dog. In fact, at some point, almost every dog will have something wrong with their skin during their lifetime. So, the better prepared you are to deal with it, the better off you are.
Hot Spots are a Hot Topic
“Our typical response to a hot spot, as a veterinarian, is to grab the clippers and shave it. And so that makes it a bit of a challenge for us to try and manage these because a hot spot needs to be treated similar to a wildfire out of the forest — you have to clear cut it. So, you have to clip out around it so that you’re an inch or two out around the hotspot into normal skin to effectively stop the spread of it. And so this is where the show dog people totally freak out because that’s that’s a year’s worth of hair coat. For some dogs that never grows back the same way.
“And this is where having a good veterinary relationship really comes into play. Your veterinarian is gonna be a lot more sympathetic to your needs and expectations if you have developed that relationship.
“It’s not that we’re unsympathetic to it, it’s just that we have to balance what your needs are with the dogs health and so that’s where this challenge comes in.
“It’s usually (caused by) a break in the skin of some kind, whether it’s an insect bite or they ran into the fence or you know, something that just dinged the skin. Allergies. Anything that causes a break in the normal integrity of the skin then allows bacteria to develop. The official name for it is an acute superficial bacterial pyoderma. It’s called a hot spot because it is hot, man. I mean, those things can spread … I’ve seen them double in size in 24 hours if you don’t get it addressed.
“You want to keep your dog healthy, their skin healthy. You want to keep them from matting. You want to be careful when you comb them or brush them that you’re not breaking the skin. That you reduce their exposure to biting insects because that can initiate it, and if they do have allergies, that you get a handle on those.
“Use your shampoos and conditioners carefully. Dilute your shampoo, rinse, rinse, rinse some more. Don’t leave any residue. You know, just be smart about how you’re taking care of your dog’s coat because if the coat is important to you, then treat it as if it’s important to you.”
Listen to the full episode to learn more on the topic of skin disorders.
570 — Breeding Theory Q&A From LIVE@5
Breeding Theory Q&A From LIVE@5
 Host Laura Reeves leads a conversation on breeding theory, replayed from a LIVE@5 live podcast from 2022.
Host Laura Reeves leads a conversation on breeding theory, replayed from a LIVE@5 live podcast from 2022.
“As we all know, dog breeding is something of, to put it mildly, a passion project,” Reeves said. “Doing it well is something we all strive for. There are some tools that we can use to accomplish that goal. No matter what type of breeding program we have, we can all use these same tools to achieve success. Sort of the theory side of breeding, reading pedigrees, breeding concepts and health testing.
“Coefficient of inbreeding is frequently shortened to COI. One of the great things is if you test both the sire and the dam of your litter, you will be able to get a predicted genetic COI based on the actual DNA. Then if you DNA test each of the puppies in your litter, you will be able to get an exact genetic DNA coefficient of inbreeding that will tell you exactly (what each puppy is). I think one of the things that many of us find sort of mind blowning is that puppies in a litter do not all have the same COI. They don’t all have the same genetics.
“And so when I did a half brother, half sister, a straight up inbreeding that I’d been planning for quite some time, and I knew what the pedigree COI was, I knew what the estimated or expected genetics COI was going to be, and I Embarked each of the 13 puppies and the actual COI in each of those puppies varied by as much as ten basis points.
“So, it’s really, really important to look at some of the tools that are now available to us. Dog breeding has always been a little bit of art and a little bit of science. Science is coming to the forefront and I don’t want us to lose the art, but I want us to be able to make good use of the science.
“Pedigree, genetic and actual COI is a very, very useful tool in our breeding program as we’re going forward. Purebred is a level of inbreeding. That’s what makes it purebred. Having a higher or lower level and how you use that and the healthy genes that you’re doubling up on or the unhealthy genes that you’re doubling up on make any enormous difference in your breeding program going forward.”
Listen in as Laura and her listeners interact on important topics from breeding theories, health testing and more.
Remember that LIVE@5 live podcasts drop on the Pure Dog Talk Facebook page the first Tuesday of every month! Join us there on March 7 for a conversation on GROOMING!
You can get more on this topic at the Dog Breeding 101 seminar.
569 – OFA Launches New Testing for Brachycephalic Breeds
OFA Launches New Testing for Brachycephalic Breeds

Dr. Kathleen Smiler, DVM, Pug Dog Club of America Health Committee Representative.
Eddie Dziuk, Chief Operating Officer at the Orthopedic Foundation for Animals, and Dr. Kathleen Smiler, DVM, Health Committee Representative from the Pug Dog Club of America, join host Laura Reeves to introduce the new BOAS testing program.
“Brachycephalic Obstructive Airway Syndrome (BOAS) is a condition which may cause breathing difficulties in breeds such as Bulldogs, French Bulldogs and Pugs,” according to the OFA. “BOAS is caused when the soft tissue in the nose and throat are excessive for the airway, partially obstructing the airway and making it difficult for them breathe normally.
“BOAS is a progressive disorder and can impair a dog’s ability to exercise, play, eat and even sleep. Clinical signs of BOAS are variable and may include noisy breathing, exercise and heat intolerance, regurgitation and dysphagia. Unfortunately, many owners are unaware of the disease, and often interpret breathing noises or difficulties as simply normal for the breed.
“In an effort to learn more about the condition, increase awareness, and ultimately reduce the incidence of BOAS, researchers at the University of Cambridge in the UK developed the Respiratory Function Grading Scheme (RFGS). The goal of the RFGS was to develop an objective test to measure the clinical diagnosis and severity of BOAS. The OFA has joined this international effort and has licensed the RFGS for use in the US and Canada.
“The exam is conducted by a specially trained and approved veterinarian and consists of 4 steps:
- A short health survey regarding the dog’s breathing history
- A brief physical exam while the dog is calm including auscultation where the assessor listens to the dog’s breathing with a stethoscope gently positioned on the side of the neck. This establishes a baseline for any clinical signs of BOAS.
- A short exercise test consisting of a brisk three minute walk. This is designed to expose clinical signs of the disease in an otherwise calm and asymptomatic dog. It is not designed to assess cardiovascular fitness.
- A post exercise auscultation after increased airway activity to compare to the pre-exercise baseline.”
“I think the veterinarians were extremely enthusiastic,” Smiler said of the veterinarians participating at a recent event in Portland, Oregon. “And I think the participants were quite pleased too, I think. I went and sat in the meet the breeds box with the pug people in Portland and everybody was quite satisfied. I think our club in general was very satisfied.”
“We examined 54 dogs (at the rollout in Portland),” Dziuk said. “We actually did 60 where we had a couple breeds that weren’t on the official breed participant list yet. So, we had 54 between Bulldogs, Frenchies and Pugs and we also had a couple of Bostons and Pekes.
“Overwhelmingly (we had) pretty good results. We had 10 Grade 0. So, the grade zeros are basically everything was good. These dogs were good breathers, they had nice wide open nostrils. There were no sounds of turbulence or anything during the auscultation, so everything was looking pretty good. We had 18 grade 1, which is also good. It means that in general, nothing could be heard without a stethoscope and you could only hear some of the minor issues with the stethoscope, but the dogs are basically still found to be clinically unaffected by BOAS. We did have 25 grade twos and we had one lone grade three.
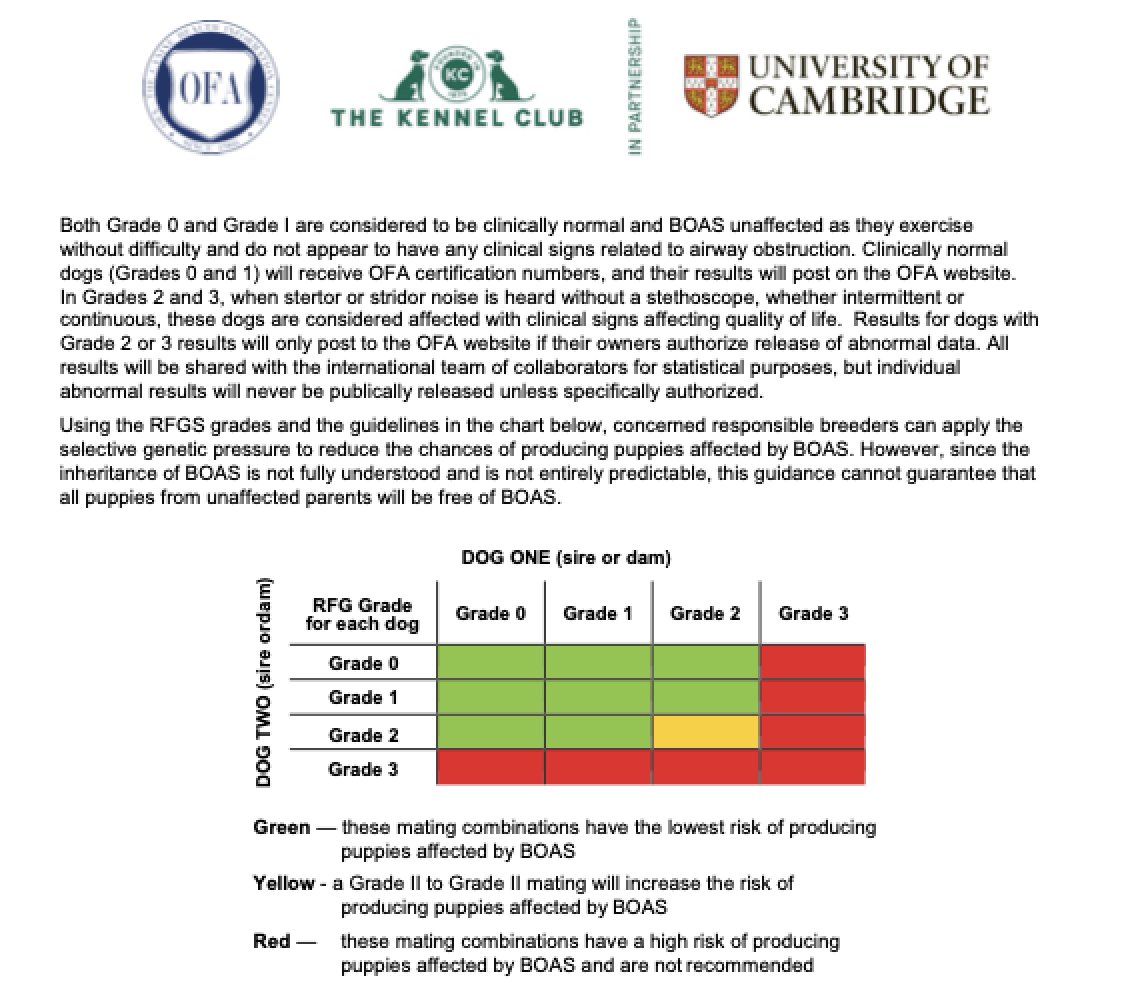 “I think that goes to prove the point that not all Bulldogs suffer breathing difficulties, not all Frenchies suffer breathing difficulties, and not all pugs do either. That there is a large group in all three of those breeds where they’re good healthy dogs that breathe fine, that don’t show signs of exercise intolerance, and we can work with those dogs and breed them and hopefully breed lots of future generations of good, healthy Frenchies, Pugs and Bulldogs.”
“I think that goes to prove the point that not all Bulldogs suffer breathing difficulties, not all Frenchies suffer breathing difficulties, and not all pugs do either. That there is a large group in all three of those breeds where they’re good healthy dogs that breathe fine, that don’t show signs of exercise intolerance, and we can work with those dogs and breed them and hopefully breed lots of future generations of good, healthy Frenchies, Pugs and Bulldogs.”
“We’re certainly very sensitive to the criticism that’s been directed toward brachycephalic breeds,” Smiler said. “I think we’re fortunate here in the US, where (breeding) isn’t a regulated activity, nor has the Veterinary Association attacked the breeds as they did in Europe. We’re going to make this information available to our members and highly encourage them (to participate). Then eventually I’d love to educate the puppy buyers. I think it’ll be very positive across the board.”
Listen in to the full episode for more details.
568 – AKC’s New Genetic Testing Program to Offer Expanded Insights
AKC’s New Genetic Testing Program to Offer Expanded Insights

Dr. Claire Wiley, VMD and her Portugese Water Dog.
Dr. Claire Wiley, Executive Director of the AKC DNA Program, joins host Laura Reeves with breaking news about the expansion of their testing capabilities.
AKC’s DNA program will soon include the option to identify traits and genetic diseases, in addition to simple parentage, Wiley announced.
“For the past 25 years, the AKC DNA program has really focused on protecting the registry,” Wiley noted. “And they did that using unique identification, kind of like fingerprints and also using those fingerprints to verify parentage. It had more of a regulatory role to it.
“A couple years ago, the AKC developed an ad hoc genetics committee. They listened to the breeders (who) were really interested in having more from the DNA program. And that’s kind of why I got hired, because we’ve listened to the feedback and are trying to bring things into the future to really serve our most important constituents, the breeder.”
Wiley, a second-generation Portugese Water Dog breeder, is a board certified veterinary specialist in Small Animal Internal Medicine. Her passion for genetic health testing started early in life after losing two PWD puppies to juvenile dilated cardiomyopathy. She later worked on the breakthrough studies to identify the genetic marker for protein losing nephropathy in Soft Coated Wheaten Terriers.
“I’m a breeder. I lived through it from the very beginning and now I’m back here to help bring the DNA program into the future,” Wiley said. “At AKC, we try to focus on all dog owners, but it all starts with the breeders who are producing the healthy dogs for all dog owners.
“The fundamental process will essentially be the same where you use a cheek swab to collect DNA and you go online to activate it. When you first go in to buy the swabs, there will be two products. The original parentage product will be called the AKC Original DNA profile and then the one that includes health tests and traits will be called the AKC Signature DNA profile.
“So when you’re actually on what we call our shop page where you’re buying the swabs, you have an option of choosing either just the Original profile, which is the $50 kit that provides parentage, or you can choose the option that still includes that $50 original profile, but also has health and traits available.
“We’re really hoping to launch this by mid 2023 at the latest, hopefully April. A lot of these companies say there are over 200 markers that they’re testing for, but if you actually talk to breeders, they’re probably focused on 2, 3, maybe 0 for that specific breed. So, we are taking the experts, you know, the Breeders, and having them tell us what we should be including as important markers for them.
“The parent clubs have what we call parent club health statement letters where they actually say this is what we are concerned about as a breed and as a group, and so we’re using those letters to determine which testing is the most important for that breed.”
Listen to the full episode for more from Dr. Wiley.
567 — Canine Bladder Stones: Diagnosis and Treatment
Canine Bladder Stones: Diagnosis and Treatment
Dr. Marty Greer, DVM joins host Laura Reeves for a deep dive on bladder stones in dogs, how to diagnose and treat them. The following information is provided by Dr. Greer.
Bladder stones are the quintessential “which came first, the chicken or the egg” question. By this, we mean that a dog can have a bladder symptoms that are caused by a bladder stone, or the bladder infection can cause bladder stones to form. Which then becomes a vicious cycle.
There are two basic types of bladder stones – the first, struvite stones associated with a bladder infection or second, any of the following other bladder stones, caused by a metabolic disturbance that causes a stone to form in the urinary tract.
How do bladder infections cause bladder stones? An undiagnosed, under-treated or recurrent bladder infection can lead to the development of struvite bladder stones. This is the most common type of bladder stone. Or another type of stone can cause irritation to the bladder which can cause a stone to form that is partly any of the types of stone below combined with a struvite stone. These form like a pearl in an oyster – the irritation of the infection or other stone type can cause a struvite coating on an existing bladder stone.
Many metabolic stones are associated with a particular breed or disease condition causing minerals to deposit in the bladder, forming stones. These metabolic stones form with long term supersaturated minerals in the urine. With time, the crystals form which develop into a bladder stone. Other factors are the pH of the urine, inhibitors and promotors of stone formation, and macrocrystalline matrix. If something like suture is in the bladder, this can also allow a stone to form.
Fortunately, most stones in the urinary tract are in the bladder itself, where they are accessible surgically. Stones in the kidney or ureter (tube from the kidney to the bladder) are not easily managed surgically or by physical removal. Stones that form in the bladder and pack together like sand in a funnel or slip from the bladder into the urethra (tube from the bladder to the outside of the body) cause urinary obstruction. This is a true medical emergency, more common in males that females due to the length and shape of the urethra, the tube from the bladder to the outside.
Males have a design flaw – their urethra is more narrow and curved, causing a greater likelihood of urinary obstruction. On the other hand, females have a design flaw, a shorter wider urethra just below the rectum that allows bacteria to ascend into the bladder, increasing the risk that a female will have a bladder infection. That infection can often lead to the formation of struvite stones.
Symptoms
Symptoms of bladder disease can be virtually non-existent to severe. The symptoms can vary:
- No signs or very subtle signs of discomfort or urinary accidents.
- Signs of blood in the urine (often not noted until there is snow on the ground or when the urine is wiped up and blood is seen on a white towel), straining to urinate, frequency of urination, inappropriate urination, +/- fever, pain, and/or urinary incontinence. Dogs are rarely “sick” with a bladder infection – they eat, drink, and act normally other than increased trips outside or urinary accidents on the floor.
- If obstructed, there will be abdominal pain, vocalizing, vomiting, dehydration, depression, heartbeat irregularities, bladder distension, in advanced cases, bladder rupture, collapse and death.
- Blood work can show elevated BUN and creatinine, kidney values if obstructed.
- Blood work may show elevated calcium if calcium oxalate stones are present.
- Blood work may show liver dysfunction in patients with urate stones.
Below is a table showing the different types of bladder stones, comparing the composition, cause, prevention and treatment options.
| Type of stone | Cause | Prevention | Treatment |
| Struvite or magnesium ammonium phosphate hexahydrate. Usually located in bladder but can be in renal pelvis. This is the most common stone in dogs at an incidence of 53%. | More common in female than male dogs, usually young dogs. Frequently multiple. Secondary to undermanaged bacterial bladder infection incl most commonly Staphylococcus spp., but less commonly seen urease-producing bacteria include Proteus spp. or Enterococcus spp. Rarely Escherichia coli, Pseudomonas spp.,
Klebsiellaspp., Corynebacterium urealyticum, or Ureaplasma/Mycoplasma spp. May have a genetic component. Breeds: American cocker spaniel |
1. Find and manage cause of recurrent bacterial bladder infection.
2. Preventive diets lower in protein, phosphorus and magnesium including: Royal Canin® Veterinary Diet Urinary SO, Hill’s Prescription Diet c/d™, Hill’s Prescription Diet w/d™, and Purina Pro Plan Veterinary Diets UR Urinary St/Ox. 3. Increased water intake 4. Weekly monitoring of urine pH and intervention if pH rises. 5. Periodic imaging for early detection of recurrence. |
1. Dissolution diet combined with appropriate long-term antibiotics. May be dissolved medically unless obstructed.
2. Acidifiers such as D,L-methionine combined with appropriate long-term antibiotics. 3. Surgical removal or Cystoscopic retrieval 4. Physical removal. |
| Calcium oxalate or calcium oxalate combined stones. Usually in the bladder but can be in the renal pelvis. 2nd most common bladder stone seen in dogs. | More common in males, middle aged.
Patients who have increased urinary excretion of calcium /or oxalate. May include Cushing’s disease, primary hyperparathyroidism, or cancer causing elevated calcium levels. Obesity. Steroid administration. Genetic predisposition. Bichon frise |
Calcium oxalate uroliths recur 8-9% after 6 months, 35-36% after one year, and approximately 50% after 3 years.
1.Diet Royal Canin® Veterinary Diet Urinary S/O Lower Urinary Tract Support, Purina Pro Plan Veterinary Diets UR Urinary St/Ox™, Hill’s Prescription Diet w/d™, and Hill’s Prescription Diet u/d™. 2.Potassium citrate orally. 3.Thiazide diuretics. 4.Vitamin B6 |
There is no known way to dissolve this stone type so must be physically removed. |
| Cystine | More common in males, young to middle aged.
Occurs secondary to cystinuria, which is caused by increased levels of cystine excreted into urine. Uncommon. Inherited mutation of SLC3A1 gene, which leads to defective amino acid transport, described in the Newfoundland, Labrador retriever, and in the cat. Missense mutation in SLC7A9 is another cause of cystinuria in the dog. Androgen-dependent cystinuria has been described in dogs. Genetic Test: DNA testing for genetic traits is available at vetGen, Penn Gen, Paw Print Genetics, DDC, Animal Genetics, and UC Davis Veterinary Genetics Laboratory in the USA, as well as Animal Genetics-UK, Laboklin, and Animal DNA Diagnostics in Europe. Breeds: American pit bull terrier |
1. Feed protein-restricted, low-sodium diet.
2. Potassium citrate to maintain alkaline urine. 3. Some patients may also require 2-MPG therapy. 4. Do not breed affected dogs, their parents, or any other offspring. 5. For breeds with androgen-dependent cystinuria, castration can help in controlling cystinuria. |
1. Low protein, low sodium, alkalizing diet: Hill’s Prescription Diet u/d™ and Royal Canin® Veterinary Diet UC Low Purine
2. Potassium citrate to alkalinize urine with a pH goal of 7.2 to 7.5 and dilute urine. 3.Physical removal. |
| Xanthine incidence 0.5 to 1% incidence of bladder stones in dogs | An uncommon type of purine urolith.
Adults 2 to 6 years of age. No sex predilection. Causes: Allopurinol administration Idiopathic, unknown |
Purine-restricted, alkalinizing, diuretic diet helps prevent xanthine recurrence including renal failure diets or ultra-low protein diets with low purine levels (Hill’s Prescription Diet u/d™ or Royal Canin® Veterinary Diet Vegetarian) may help. Add water to food to keep urine dilute. Use potassium citrate may be needed to keep urine pH alkaline. | Will not dissolve. Must be physically removed.
Stop allopurinol treatment if possible. |
| Silica incidence 0.9% of canine bladder stones | Incidence world-wide seems regional. Primarily male dogs. Usually 6 to 8 years of age.
May be genetic with German Shepherds, Labradors, Golden Retrievers and Old English Sheepdogs being over-represented. Cause unknown.
|
Monitor with urine testing and imaging to check for recurrence. May help to feed more animal protein and less vegetable protein to reduce recurrence. Feeding diets higher in animal protein and lower in plant-based proteins (such as soybean, rice, corn gluten feed, oat-based cereals) may be beneficial. Increasing water intake may help decrease silica concentration in urine. Do not allow patients to eat grasses and soils with higher silica content. | No dissolution therapy known.
Must be physically removed. |
| Calcium phosphate – incidence 1 to 2% of canine bladder stones | Brushite more common in males.
Breeds predisposed include Shih tzu Lhasa apso Miniature Schnauzer Yorkshire terrier Miniature poodle Pomeranian Bichon frise American Cocker Spaniel |
Identify and treat the underlying cause such as primary hyperparathyroidism or Cushing’s diease (hyperadrenocorticism). Keeping urine pH of 6.5-7.5 and urine dilute helps reduce risk of recurrence. Ideal preventive diet is unknown; diets aimed at preventing calcium oxalate uroliths are reasonable options. | Associated with primary hyperparathyroidism or Cushing’s disease (hyperadrenocorticism). These also may occur as part of stones that are largely composed of struvite or calcium oxalate. Associated with alkaline pH. |
| Urate incidence 5 to 8% of canine bladder stones | Either sex, usually young dogs. Uric acid and its various salts. Associated with liver disease, hepatic dysfunction, portosystemic shunts, inherited, or less commonly, caused by urinary tract infections (UTI) with urease-producing bacteria.
Genetic mutation in the SLC2A9 gene: Australian shepherd |
Frequently recurrent at rates of 33 to 50%.
Annual or biannual imaging with ultrasound or x-rays to monitor. |
1. Dietary therapy with low purine diets (eggs, dairy and vegetable protein) – may be dissolved medically unless obstructed: Hill’s Prescription Diet u/d™, Royal Canin® Veterinary Diet Canine Vegetarian, and Royal Canin® Veterinary Diet Urinary UC Low Purine.
2. Potassium citrate at 50-150 mg/kg PO q 12 hrs or sodium bicarbonate at 25-50 mg/kg PO q 12 hrs may be used. Avoid pH above 7.5 3. Allopurinol 4. Physical removal 5. Managing underlying liver disease. |
| Combination stones | Any combination of the above stones can occur. The largest % component is reported when there are several mineral components to the stone. | Based on analysis | Based on analysis |
| Dried solidified blood | Cats only |
The above table is a summary of information published on www.veterinaryinformationnetwork.com. Thanks to this author Kari Rothrock DVM.
Diagnosis
- Symptoms are noted.
- Urinalysis: crystals seen on microscopic evaluation of the urine, bacteria, white blood cells, and white blood cells seen under the microscope.
- Culture – to identify the causative bacteria.
- X-rays – seeing stones in the bladder, kidney, ureter or urethra. May require contrast x-rays.
- Ultrasound – stones or gritty material seen blocking the ultrasound beam on ultrasound. This may be described as a “snow globe”.
- Stone analysis – essential to know the cause and how to try to prevent formation of future stones.
- Cystoscopy – when an endoscope is passed into the bladder to look for stones. Removal may be achieved at this procedure.
Physical Removal of stones: there are several techniques available to remove stones from the urinary tract.
- Surgical removal – is a procedure available at most small animal veterinary clinics with basic surgical availability. If an obstruction is present, immediate surgical intervention is essential.
- Cystoscopic retrieval – requires an endoscope and special baskets to retrieve stones from the urethra and/or bladder.
- Voiding urohydropropulsion – With sedation or anesthesia, the bladder is catheterized, filled with fluids multiple times, and with pressure on the bladder, efforts to push the stones out through the urethra is attempted. This works best in small dogs with small stones.
- Extracorporeal Shock Wave Lithotripsy (ESWL) – This involves using a shock wave to a patient immersed in a water bath. Bladder stones may move too much for this to have a successful outcome so is better suited for stones in the kidney or ureter.
- Laser lithotripsy – This involves using a laser to fragment them, then the fragments are removed. This works better in female than male dogs. Small dogs and large bladder stones may not lend themselves to this treatment option.
- Retrograde Urohydropropulsion (RU) – this involves flushing stones from the urethra back into the bladder for removal. In general, the patient will require sedation or anesthesia, followed by removal of some urine to relieve the pressure on the bladder.
Other than surgical removal, the others are usually only available at larger referral centers or veterinary schools.
Dissolution – is a process by which bladder or kidney stones can be dissolved using special diets, drugs, and or antibiotics. Not all stone types will dissolve. And not all dissolvable stones will dissolve safely. If the dog has an obstruction and cannot urinate, immediate physical removal of the stones is essential as urinary obstructions are life-threatening. Not all dogs will eat the diet required to dissolve the stones. Not all owners are willing or able to administer the medications and diets necessary to dissolve the stones. Frequent monitoring of the size and location of the stone is essential to safely allow stones to dissolve. The required diets are prescription diets, and the medications are also prescription drugs. Care in selecting the correct food and medication is required, thus the reason for prescriptions from the pet’s veterinarian.
Prevention can often be successful. Again, this requires that the owner(s) of the dog take great care to provide plenty of fresh water frequently, let the dog out to urinate frequently, and administer medication and food without “cheating”. Owners may also need to check weekly urine samples to assess the urine pH for early adjustments in medication and food to prevent recurrences.
As a result, a mutual treatment plan with the pet owners and their veterinary team is essential for a successful outcome.
566 – Routines Create Coping Skills in Traumatic Times
Routines Create Coping Skills in Traumatic Times

Dr. Angel Iscovich, MD, author of “The Art of Routine”
Dr. Angel L. Iscovich, M.D. joins host Laura Reeves to talk about creating routines as a coping mechanism in traumatic times. An emergency room physician and Miniature Schnauzer enthusiast, Iscovich’s book “The Art of Routine” has great suggestions as we emerge from the trauma of the pandemic years.
Iscovich studied older patients and found that consistently, folks who lived well into their older years had one thing in common. Routines. Even routines that aren’t necessarily “healthy” were beneficial, Isocvich noted.
“I noticed people that were over 100 years of age, centenarians, I noticed two qualities that they had,” Iscovich said. “One is that they have a stable environment. By that I mean both physical and people around them. And two, they had a very, very regular routine. They had a rhythm, a routine, things that they did with great regularity.
“But what I also noticed is what they did varied quite a bit. So, some of them were doing not necessarily healthy things, but that got me to thinking. That may be part of the key is more the *how* than the *what* we’re doing. In other words, the routine may be more important than actually what you’re eating because here’s this 100-year-old having Dr. Peppers every day, you know, and that doesn’t seem like the right thing to do, but that there was something to the fact that you had routine and regularity.
“It seemed to me that for us as humans in this world where we’re using our digital world as we are today in computers and sort, that we’re being constantly interrupted and disrupted and being always tempted to do different things all the time, and that maybe, maybe changing things up too much is not really the way to go.
“We seek and survive by having kind of stability. Homeostasis is what it’s called in some of the physiological terms. And having equilibrium.”
Iscovich’s suggestions for building routine for a healthier outcome:
- Recreate your own routine
- Get more exercise
- Get outdoors
- Do daily affirmations
- Quiet time … get rid of the sensory input
- Self discipline… dopamine works. Do one event, do it repetitively, complete the smallest task. This makes the body and brain chemistry give you a good feeling. Stick with one thing. This stabilizes us in times of uncertainty
565 – Bumble’s Story: Behind the Scenes with Donna Beadle
Bumble’s Story: Behind the Scenes with Donna Beadle
Donna Beadle joins host Laura Reeves to share the epic, joyous and eventually tragic story of Bumble the Berger Picard.

Bumble, in his glory days as the #1 Owner Handled Berger Picard, with Donna’s husband, Mike Beadle.
Bumble was lost for 10 days in the high desert of Wells, Nevada. Donna shares the lessons she learned, the emotions, the hardships, the dark humor, the kindness of strangers as well as her heartache, hope and second guessing, tips and suggestions for others in similar situations.
“If you are looking for a lost pet, especially in an area you don’t know, hire a professional,” Donna said. “They are a wealth of information. I know a lot about dogs, but I don’t know anything about lost dogs. They came they brought their trap, advised me about getting stuff out in the community. Not everybody is on social media, lost dog signs are hugely important.
“There were sightings on and around I80, which was terrifying, but that’s where we were focusing our efforts. I had to drive that interstate every day looking for my dog’s body…”
Donna traveled from Minnesota to Nevada at the first news of Bumble’s loss. She and a team of trackers, trappers, local residents, co-owners and dog community spent almost a week hunting for Bumble. After losing hope with no sightings and the tracker hitting a dead end on the trail, she returned home.

Juan, the ranch worker who first sighted Bumble, gave up his day off to help on the search and was instrumental in Bumble’s reunion with Donna.
A sighting by a ranch worker the next day brought her flying back for three more days of searching in a new area.
“Why signage and flyers are so important, the ranch owner and the ranch worker’s daughter both called because Juan saw ‘the dog in the picture,’” Donna said.
More traps, trappers and local folks restarted the search a mile back on the ranch land.
It was like looking for a needle in a haystack
Strapped into unfamiliar snowshoes, Donna traipsed through sagebrush and waist-high snow drifts in an area that they’d found new tracks in the snow. Juan, the ranch worker, came out on his day off to help with the search.
By a miracle, Donna glanced up to see her dog huddled under a small sagebrush.
Donna said, “OMG, I’ve stumbled upon Bumble.”
She was able to get a hand on him through a careful approach. He was so weak she had to carry him out. While a bodybuilder, Donna isn’t accustomed to the 6000+-foot elevation of the high desert and struggled through snow drifts until a vehicle was able to reach them.
Bumble was raced to the veterinarian, and given emergency treatment, care, and love. The extreme stress on his body caused him to crash four days later and, tragically, he couldn’t fight any longer.